The Texas Tech chemical engineering researcher who formed a COVID-19 rapid test evolved the same concept into a device that can not only identify but monitor the virus.
It’s about the size of the tip of a pen, but the invention could become a breakthrough for millions worldwide.
This novel electrochemical biosensor allows for rapid human immunodeficiency virus (HIV) detection in saliva in less than 15 minutes using nickel-based electrocatalysis. It’s the latest non-invasive virus sensor developed by the lab of Gerardine “Gerri” Botte, chemical engineering professor and Edward E. Whitacre Jr. College of Engineering Endowed Chair in Sustainable Energy.
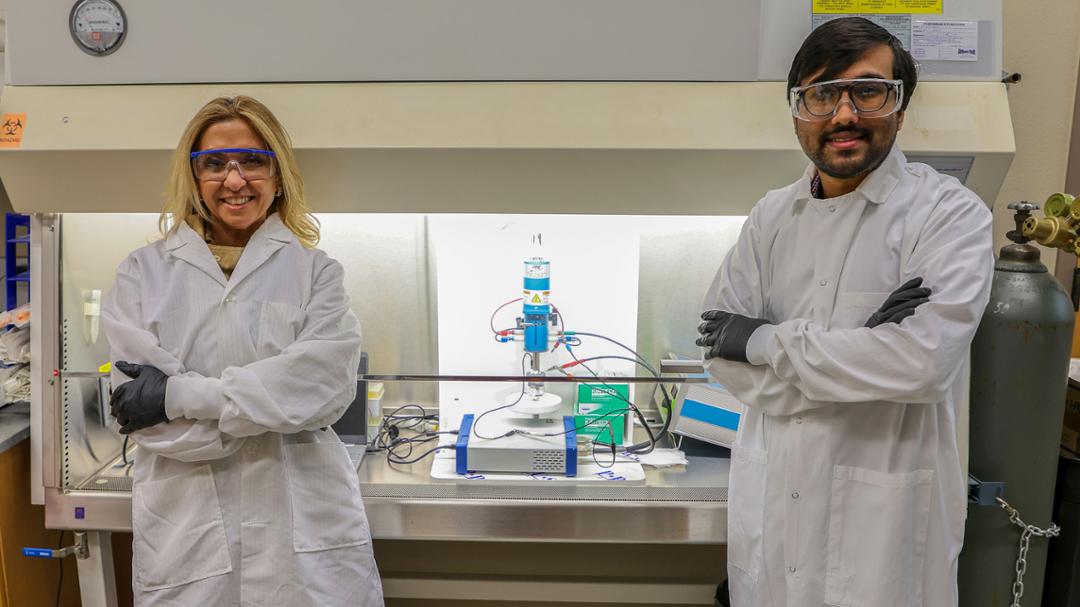
Botte and her team made headlines during the 2020 pandemic for creating an ultra-fast COVID-19 detection sensor that was as accurate but faster than rapid tests available at the time. Inspired by the same technique, she decided to collaborate with her former graduate student Ashwin Ramanujam, an innovation manager at the University of Maryland, and Dipu Saha, a fourth-year chemical engineering doctoral student.
The researchers were able to successfully evolve the sensor platform post COVID-19 into an innovation that can detect HIV p24 protein in saliva with unprecedented sensitivity – addressing a critical gap in early HIV diagnosis. The virus can lead to acquired immunodeficiency syndrome (AIDS) – an ongoing and chronic condition – but quick detection is one way to minimize the spread of AIDS.
“When we came up with the COVID-19 test, I said, ‘This will be a piece of Texas Tech University’s heart everywhere in the world,’” Botte recalled. “And now with this HIV test, I think there is more evidence that it will not only impact society significantly but also bring Texas Tech worldwide recognition. So, I’m very excited about that.”
Botte believes this biosensor is a significant step toward much-needed accessible HIV detection, since current testing methods cannot reliably detect HIV in saliva samples due to the low concentration of viral particles in oral fluid.
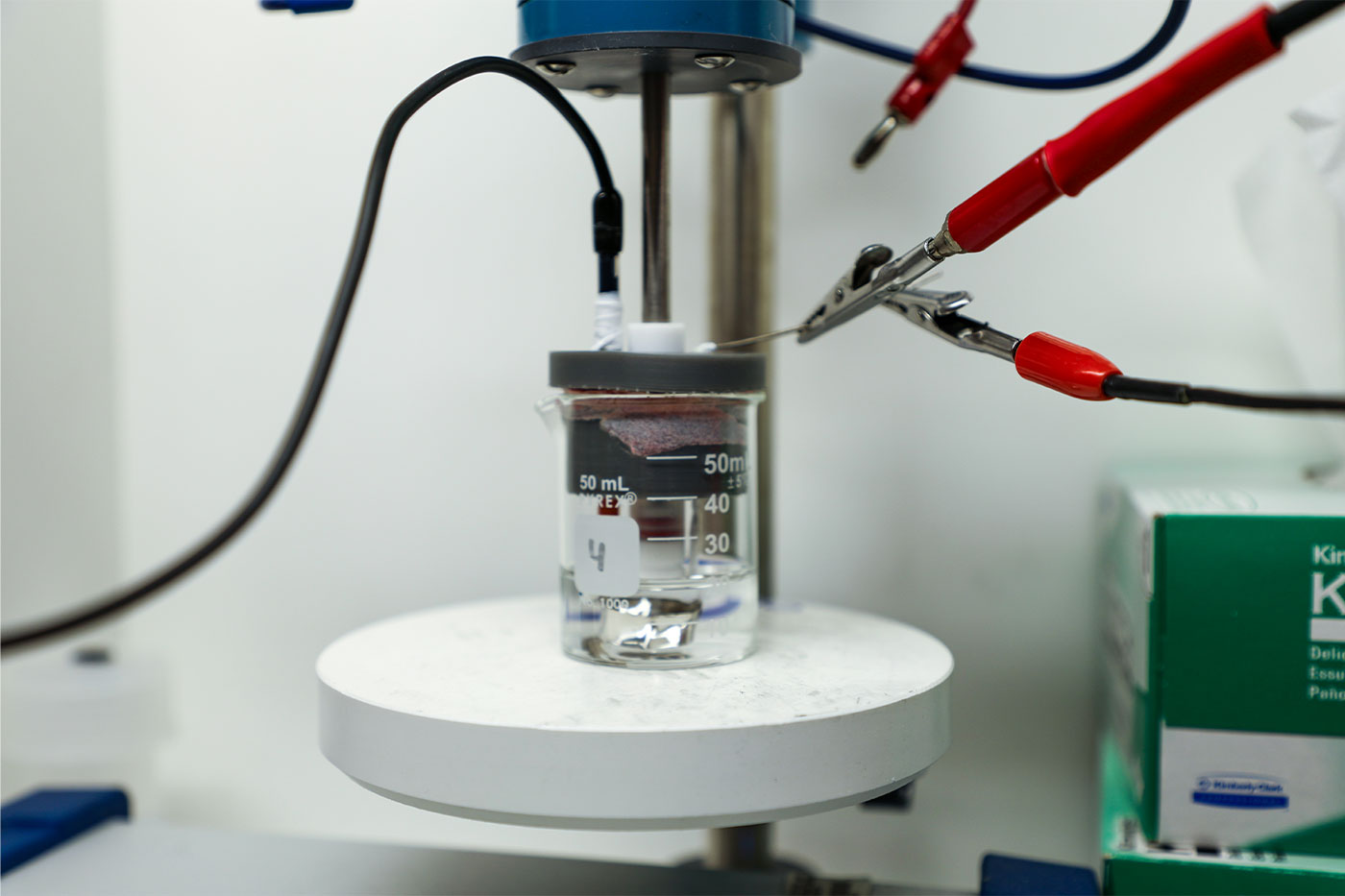
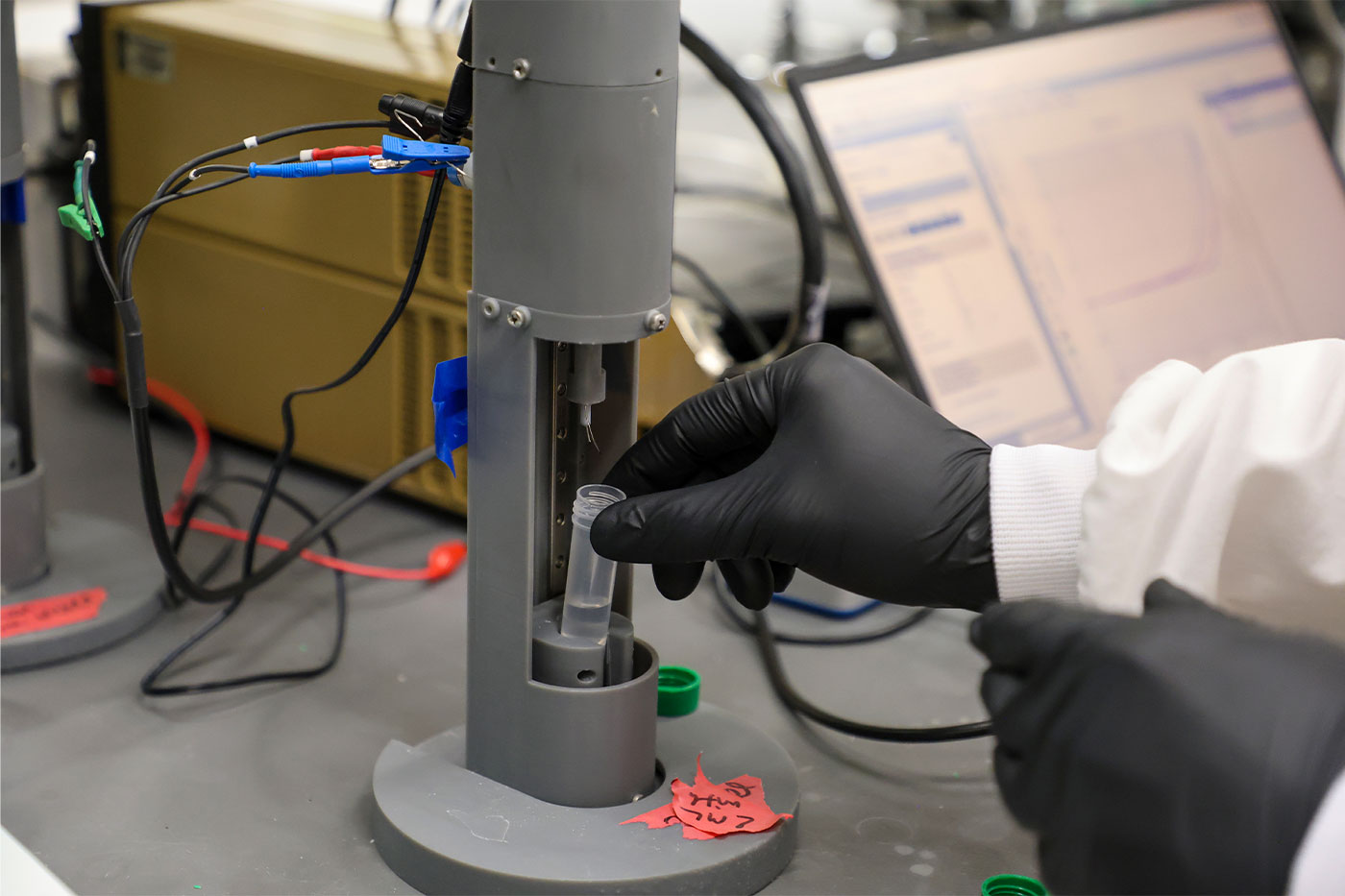
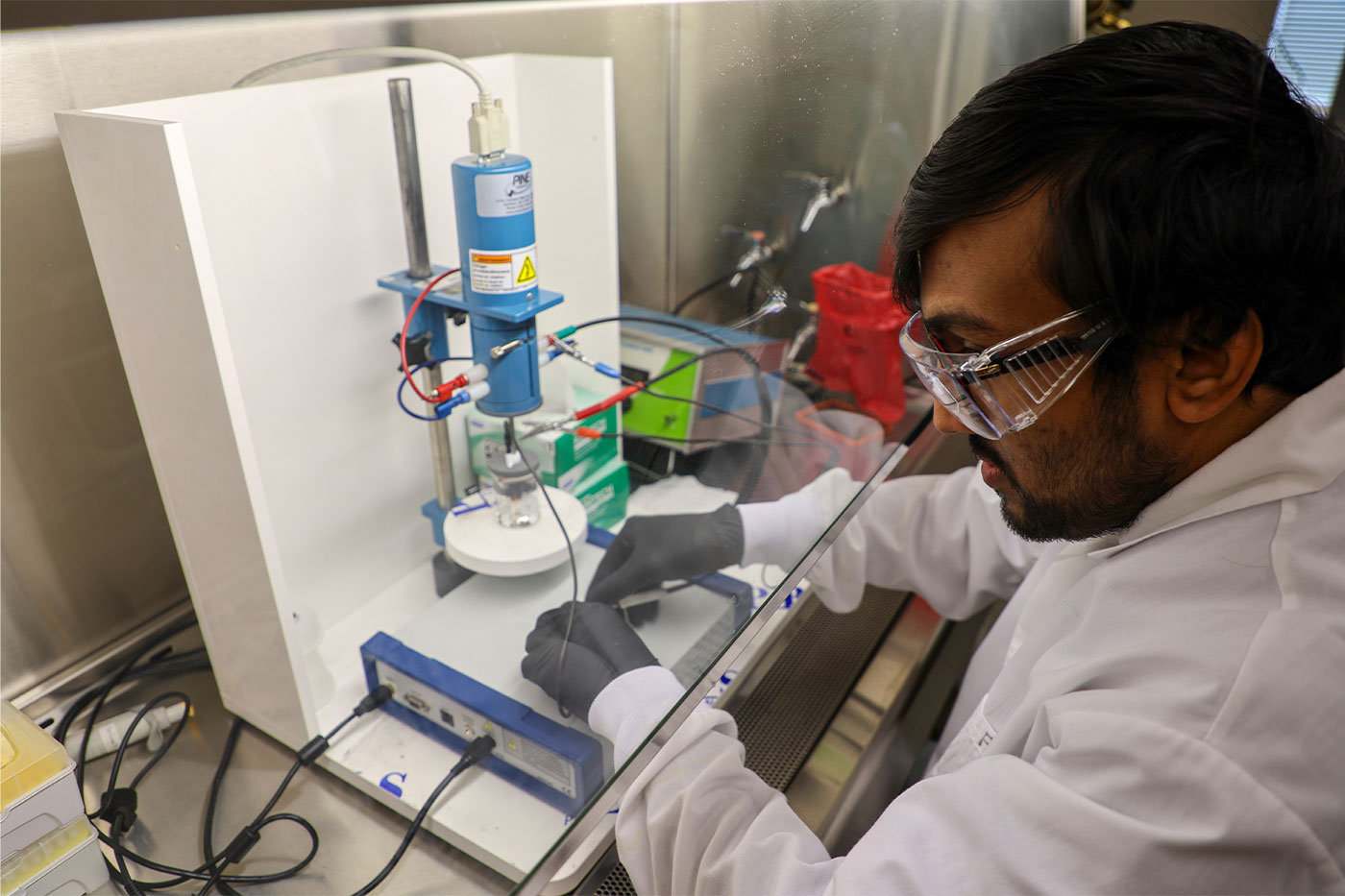
She explains the test developed in her lab can be done by anyone with any background as the sensor is submerged in a buffer solution smaller than a coffee mug to detect proteins that break from the HIV virus. The results of the test can enable patients to monitor the effectiveness of their treatment.
"My understanding is people who have HIV can live life through medications that exist, but what happens is when the medication stops working, their viral count goes back up,” Botte explained. “So, the test will also be able to track how your treatment is going in a way that could be very fast compared to what exists today.”
The biosensor’s simple and cost-effective design and function required a year-and-a-half of trial-and-error efforts by Saha, who performed tests with costly saliva from HIV patients.
Once the team strengthened their hypothesis of why the HIV sensor was effective by comparing it to the different performance of protein groups in two other viruses like influenza, they published their findings in December 2024 in “The Electrochemical Society.”
Botte shared the news on LinkedIn shortly after and received more than 2,000 impressions within the first hour.
“Some of the comments were about how revolutionary this work is and the impact to society and certain communities,” she remembered. “Some other feedback was, ‘Thanks for inspiring us to do things like this,’ so I think it inspired the scientific community to look at potential opportunities people didn’t think about before.”
The positive response has Botte proud of the work Saha dedicated to this project.
“It was a very hard scientific challenge,” she said. “I had the tendency to push him to do more and more, and I think now he feels that confidence and is super excited about how our persistence and creativity changed the paradigm of a certain area.”
Likewise, Saha is grateful to Botte for the opportunity to develop the biosensor. He came to Texas Tech from Bangladesh with hopes to contribute to society through research, and his work with the HIV sensor enabled him to achieve that.
“Dr. Botte had the idea and told me to go for it,” he said. “Whenever I needed something, I just talked to her and she was very kind and helpful.”
The team’s work is not over yet, though. They remain focused on miniaturizing and increasing the sensitivity and selectivity of the HIV sensor.
Once these milestones are achieved, they will be ready to approach commercializing the technology.
“We want it to reach everywhere in society, and I believe this device could potentially have a significant impact in many other countries,” Botte said. “But that is going to be highly dependent on investment and grant funding.”
Botte remains optimistic about the support her team will receive moving forward, particularly through the Office of Research Commercialization, which has provided significant aid throughout her research endeavors.
She believes the COVID-19 and HIV tests are just a few of the innovations that will emerge from her lab in the coming years.
“We’re evolving in other areas,” she shared. “Right now, I have a student who is following up on breast cancer. So, I hope that potentially, a year from now, we can announce that we developed a method to monitor breast cancer in saliva samples. It makes me excited to continue to inspire the students to make an impact.”